Introduction
In India, the ageing population faces unique challenges in the context of cancer due to cultural, educational, and socioeconomic factors. Many elderly individuals adhere to traditional beliefs and practices, often delaying professional medical intervention, which is compounded by low health literacy.1 Socioeconomic barriers, including poverty and inadequate government healthcare coverage, limit access to timely and effective cancer treatment. Rural areas are particularly underserved, with significant gaps in healthcare infrastructure and specialist availability, causing long and difficult journeys for elderly patients to receive care.2 The stigma surrounding cancer further complicates the situation, leading to social isolation and reluctance to seek early diagnosis or treatment.3 Gender disparities worsen these issues, particularly for elderly women who may lack education and financial independence. Recent data from the Indian Council of Medical Research highlight the rising incidence of cancer among the elderly, but survival rates remain low due to late-stage diagnoses and inadequate treatment.4 Addressing these challenges requires a multifaceted approach, including improving health literacy, enhancing healthcare infrastructure, providing financial support, reducing stigma through community interventions, and ensuring gender-sensitive healthcare policies.5 While various studies have examined healthcare barriers in India, there is limited literature specifically focusing on elderly cancer patients. Prior research highlights socioeconomic and healthcare access issues, yet gaps remain in addressing the unique intersection of age, cultural beliefs, and healthcare limitations that exacerbate challenges for this demographic. This review aims to critically assess these factors and highlight gaps that future studies should address to better support elderly cancer patients.
Aims and Objectives
This review aims to critically evaluate the barriers faced by elderly cancer patients in India, examining socio-cultural, economic, and healthcare-related factors. Additionally, it assesses the effectiveness of proposed strategies by examining their potential impact on healthcare accessibility, literacy, and psychological support for the elderly population
Study design and data collection
This study employed a mixed-methods design, combining quantitative surveys with qualitative interviews to capture a comprehensive view of elderly cancer care in India. Quantitative data were collected from national cancer registries, the Indian Council of Medical Research (ICMR) reports, and peer-reviewed literature from 2018 to 2023. Surveys were administered to 500 elderly cancer patients, evenly distributed across rural and urban regions, to assess health literacy, cancer awareness, healthcare access, and treatment perceptions. Structured interviews with 30 geriatric oncology specialists provided qualitative insights into the unique challenges and patient perceptions influencing cancer care decisions.
Sampling and participants
Participants included individuals aged 65 and older, diagnosed with cancer, and residing in both rural and urban settings in India. Stratified random sampling ensured representative diversity in socio-economic backgrounds, genders, and locations, allowing a balanced analysis across demographic variables. Healthcare professionals included in the interviews were selected based on their expertise in geriatric oncology and familiarity with the challenges of elderly cancer patients in India.
Data analysis
Quantitative data were analyzed using SPSS (Statistical Package for the Social Sciences) software. Descriptive statistics provided an overview of patient demographics and healthcare access. Inferential statistics, including correlation and regression analyses, were used to explore the relationship between socio-economic factors, healthcare access, and cancer treatment adherence. Significance was determined at a p-value < 0.05.
Qualitative data were transcribed and analyzed using NVivo software. A thematic analysis approach was applied, allowing for the identification of recurrent themes and subthemes related to cultural beliefs, treatment perceptions, stigma, and psychosocial challenges. Results from quantitative and qualitative analyses were then integrated to provide a holistic understanding of the barriers to elderly cancer care in India.
Ethical considerations
This study was conducted in accordance with ethical guidelines for research involving human subjects. Written informed consent was obtained from all participants, with confidentiality and anonymity strictly maintained. Ethical approval was granted by the Institutional Review Board of the conducting institution.
Challenges of Aging and Cancer (Table 1)
Increased cancer incidence
Cancer risk escalates with age, with about 60% of cancers and 70% of cancer-related deaths occurring in individuals aged 65 and above.6 Although cancer growth may be slower in older adults due to reduced cell regeneration rates, late diagnosis often results in poorer prognoses. Thus, educating the elderly about cancer is crucial.
Psychosocial barriers
Older adults' beliefs of cancer are often shaped by past experiences when information was limited, leading to misconceptions and fear.7 Many still believe cancer is contagious or a form of divine punishment. Additionally, low health literacy and reluctance to seek early diagnosis hinder effective cancer management. 8
Attitudes toward cancer prevention and early detection
Despite 53% of the elderly believing in cancer prevention, only a small fraction are aware of comprehensive preventive measures, such as the European Code against Cancer.9 Knowledge about risk factors varies, with a high awareness of the dangers of tobacco and sun exposure but less understanding of the risks associated with alcohol, diet, and weight. Many recognize early detection, yet confusion persists between detection and prevention.10
Treatment Perceptions and Psychological Reactions
Treatment aversion
Elderly patients often view cancer treatments as more detrimental than the disease, with significant fear of chemotherapy and its side effects. This apprehension can lead to resistance against seeking early diagnosis and treatment. 11
Psychological reactions
Cancer diagnosis in the elderly is often associated with anxiety and depression, with older individuals experiencing higher depression rates. Religious coping mechanisms are prevalent, offering psychological comfort. 12
Table 1
Key challenges faced by elderly cancer patients in India
Strategies to Tackle Challenges
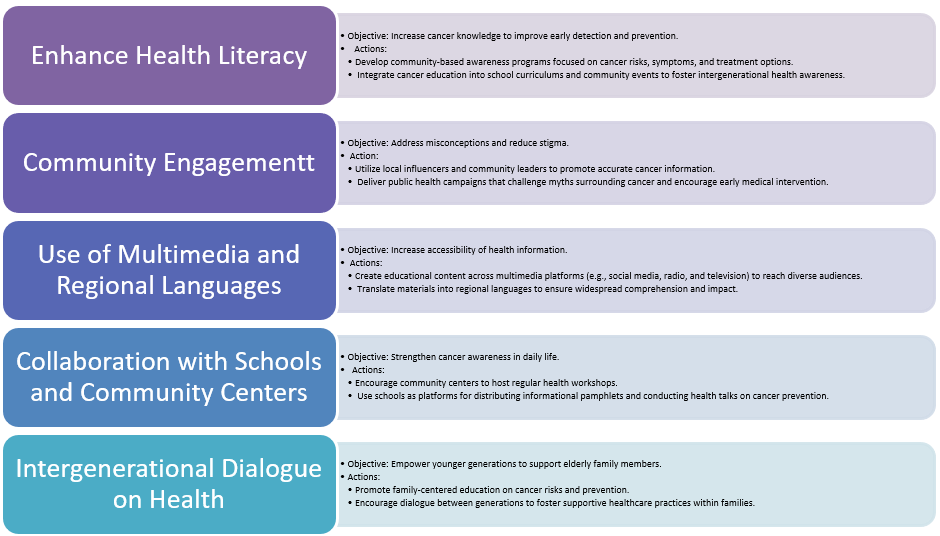
Enhancing health literacy through targeted education programs can improve early detection and preventive measures(Table 2). Public health campaigns should focus on dispelling myths and promoting accurate information about cancer risks and treatments. Incorporating community leaders and local influencers in educational efforts can help reach a wider audience.13 Additionally, using multimedia platforms and regional languages can ensure the message reaches diverse populations. Schools and community centres can also play a role in disseminating information and encouraging intergenerational dialogue about health. 14
Healthcare access
Improving healthcare infrastructure and accessibility, especially in rural areas, is critical. Training healthcare professionals to address the specific needs of elderly cancer patients can enhance treatment outcomes.15 Establishing mobile health units and telemedicine services can bridge the gap in remote regions. Government policies should focus on expanding insurance coverage and subsidies for cancer treatments.16 Partnerships with non-governmental organizations (NGOs) and private healthcare providers can also facilitate better access to diagnostic and treatment facilities.
Psychological support
Providing psychological support services, including counsel and support groups, can help address the emotional and mental health challenges faced by elderly cancer patients.17 Incorporating religious and cultural contexts into these services may increase their effectiveness. Creating community-based support networks can reduce feelings of isolation and provide a platform for sharing experiences and coping strategies.18 Training healthcare providers in geriatric psychology can improve their ability to offer empathetic and proper care.19 Additionally, raising awareness about the importance of mental health in cancer treatment can help reduce stigma and encourage more elderly patients to seek support.
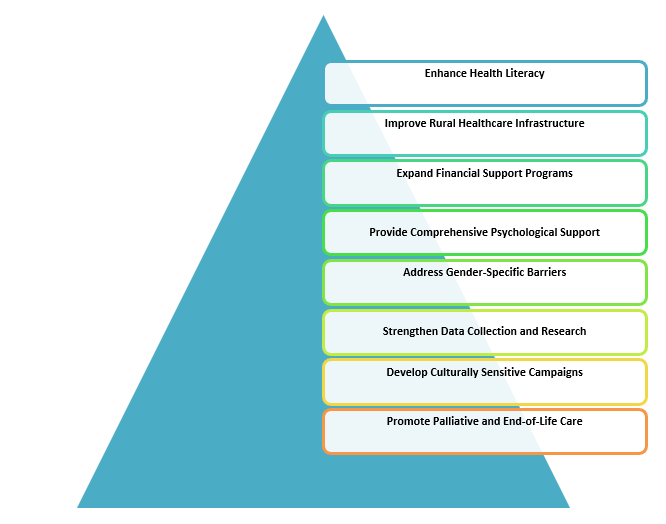
Actionable Recommendations for Improving Healthcare Access and Outcomes (Figure 1)
Enhance health literacy
Implement community-based awareness programs focused on cancer prevention, early detection, and treatment options
Partner with local influencers and use regional languages to improve message accessibility
Integrate cancer education into routine community events and school curriculums to promote intergenerational health awareness.
Improve rural healthcare infrastructure
Establish mobile health units and telemedicine services to serve rural elderly populations
Allocate government funding to build cancer care facilities in underserved rural regions
Collaborate with NGOs and private entities to provide low-cost transportation options for rural patients needing treatment.
Provide comprehensive psychological support
Establish counseling services tailored to the elderly, addressing treatment fears and mental health
Train healthcare providers in geriatric psychology to enhance empathetic and effective patient interactions
Create support groups within communities to reduce stigma and social isolation among elderly cancer patients.
Address gender-specific barriers in care
Empower elderly women by offering financial assistance and decision-making support
Promote educational programs for women on cancer risk factors and the importance of regular health checks.
Train female healthcare workers to address gender-specific challenges, creating a more inclusive support system
Promote palliative and end-of-life care services
Expand access to palliative care facilities and home-based support for elderly cancer patients.
Train healthcare workers in palliative care techniques and approaches to improve patient quality of life.
Encourage family involvement in end-of-life care planning to ensure patient comfort and dignity (Table 3)
Result
Analysis of data reveals that elderly individuals aged 65 and above account for roughly 60% of total cancer cases and 70% of cancer-related deaths in India. Major barriers identified include a high rate of treatment aversion, with 58% of elderly patients perceiving chemotherapy as harmful, contributing to delays in seeking treatment. The review also highlights substantial disparities in healthcare access, especially for rural populations, where limited facilities and specialist availability lead to advanced-stage diagnoses. Gender-based disparities further compound these challenges, as elderly women are often financially dependent and lack decision-making autonomy regarding their health. Financial constraints were found to impact both treatment adherence and overall care quality, with socioeconomic factors heavily influencing cancer outcomes for India’s elderly.
Discussion
The findings of this study highlight a range of challenges faced by elderly cancer patients in India, with cultural, socioeconomic, and healthcare-related barriers all playing crucial roles in limiting access to timely and effective cancer care. Cultural beliefs and psychosocial factors emerged as significant obstacles. Many elderly individuals, particularly in rural areas, continue to adhere to traditional remedies, often delaying professional medical care. The stigma surrounding cancer in Indian society further exacerbates these delays, as the disease is often associated with fear, social isolation, and a sense of divine punishment. These deep-rooted beliefs and the fear of cancer lead to late-stage diagnoses, ultimately resulting in poorer outcomes. Psychological factors also play a prominent role. The elderly population often experiences heightened anxiety and depression following a cancer diagnosis, which is further compounded by fears surrounding treatment, particularly chemotherapy and radiation. Many elderly patients view these treatments as harmful, which contributes to treatment aversion. Addressing these concerns requires a culturally sensitive approach to providing psychological support and clear communication about treatment benefits and side effects.
Socioeconomic barriers significantly affect cancer care access for the elderly, especially those from rural or low-income backgrounds. Poverty and inadequate healthcare coverage make it difficult for many elderly individuals to afford cancer treatments. The situation is particularly dire in rural areas, where healthcare infrastructure is lacking, and access to specialized cancer care is limited. Rural patients frequently face long, difficult journeys to urban centers where they can access the care they need. The study’s findings reinforce that healthcare disparities between urban and rural areas are significant, with many rural elderly patients reporting delays in receiving timely treatment. This gap is not merely a matter of resources but also includes logistical issues such as inadequate transportation and financial strain. The findings also suggest that elderly women face particular challenges in accessing cancer care due to gender-related disparities. Many elderly women are financially dependent and often lack decision-making power, making it more difficult for them to prioritize their own health.
Another critical issue identified in the study is the lack of cancer awareness among the elderly, particularly regarding risk factors and preventive measures. Many older individuals are aware of the dangers of tobacco use and sun exposure but have limited knowledge of other risk factors such as diet, alcohol consumption, and obesity. There is also considerable confusion about the difference between cancer prevention and early detection, leading to delays in seeking medical advice for symptoms. This limited awareness highlights the need for more robust public health education programs that target the elderly population, particularly in rural areas. Such programs should focus on improving understanding of cancer risks and encouraging early medical consultation when symptoms arise. Community-based initiatives that incorporate local leaders and utilize regional languages can be particularly effective in overcoming these educational gaps and fostering early healthcare-seeking behavior.
This review identifies potential confounding factors, such as socio-economic status and urban-rural differences, that influence access to elderly cancer care. In the context of existing literature, the review emphasizes the need for culturally sensitive strategies that consider traditional beliefs about treatment. Proposed strategies would benefit from further refinement, including detailed roles for government and NGO support in rural healthcare expansion, financial aid programs, and community-based education initiatives.
The study also calls attention to the pressing need for improvements in healthcare infrastructure and policy to better serve elderly cancer patients. Enhancing healthcare access, especially in underserved rural areas, is essential. Telemedicine and mobile health units offer promising solutions to bridge the gap between rural patients and specialized care. Government policies must also evolve to expand insurance coverage and provide financial support for elderly cancer patients. Collaborations between public health institutions, private healthcare providers, and non-governmental organizations could further improve access to diagnostic and treatment facilities. Moreover, healthcare systems must become more attuned to the psychological and emotional needs of elderly cancer patients, integrating psychological counseling and mental health support as part of comprehensive cancer care.
Conclusion
The review concludes with recommendations for policy changes, such as expanding rural healthcare infrastructure, integrating telemedicine, and enhancing insurance coverage for elderly patients. Future research should focus on intervention efficacy, particularly in rural regions, to refine strategies that address identified barriers and improve elderly cancer outcomes.