Introduction
In abdominopelvic oncology, PET/CT has long been regarded as a cornerstone because it allows for thorough staging and restaging using a variety of radio pharmaceutical agents. Nevertheless, there are restrictions on the collection and analysis of PET/CT data. These include the inability to collect PET and CT data simultaneously and the restricted assessment of soft tissues as a result of the custom of obtaining a noncontrast CT scan for anatomic localization. It is commonly known that using numerous pulse sequences during abdominal and pelvic MRI, either with or without intravenous contrast material delivery, improves soft-tissue characterisation.
An developing imaging technique called PET/MRI was originally authorized for use in clinical settings and has since been progressively incorporated into clinical practices. By combining the improved soft-tissue characterisation provided by MRI with simultaneous PET image collection, PET/MRI allows for the precise localization of anatomic structures and gets around some of the drawbacks of PET/CT. In this post, I describe the fundamental technical features of PET/MRI, its benefits and drawbacks when compared to PET/CT, and how this modality is used for a variety of cancers in pelvic oncology, including prostate cancer.
PET/MRI versus PET/CT
Around the world, PET/CT is a commonly available imaging modality that is frequently utilized for staging and restaging a variety of cancers. For the diagnosis and treatment of different malignancies, PET/CT systems are covered by a number of National Comprehensive Cancer Network guidelines and have specific protocols and criteria. On the other hand, PET/MRI is a relatively new imaging modality that has not yet been included in the imaging criteria for many malignancies, while offering some potential advantages over PET/CT.
PET/MRI systems provide the opportunity to perform standard-of-care staging imaging in a single setting (e.g., brain MRI for patients with advanced-stage melanoma or lung cancer) as well as whole-body and regional imaging in a single session, which may be advantageous in the setting of certain cancers (e.g., prostate and rectal cancers). Additionally, compared to PET/CT, PET/MRI uses less ionizing radiation. Younger patients who may require several PET exams over the course of their disease might benefit from this.1
Furthermore, PET data unique to a place can be obtained while acquiring MR images. Compared to a whole-body PET imaging bed assessment, which has been demonstrated to increase minor lesion detection and characterisation, this site-specific PET picture acquisition frequently takes longer.2 Regional MRI-based PET/MRI exams can take longer to acquire images, which may not be comfortable for some patients or those who are claustrophobic. This restriction can be somewhat addressed, though, by streamlining and streamlining processes to address important clinical queries by utilizing synergistic data from both the PET and MRI pictures. Although PET/MRI will never overtake PET/CT as the mainstay of molecular oncologic imaging, it may be useful in a few specialized applications related to pelvic oncology.
Advantages and Disadvantages of PET/MRI
It is critical that medical practitioners understand the possible benefits and drawbacks of PET/MRI imaging. Radiotracer uptake in the pelvis and better characterisation of soft tissues are generally provided by PET/MRI. For instance, using PET/CT to image the uterus and endometrium might be difficult since physiological activity in these regions can mimic cancerous growths. With PET/MRI, it is significantly simpler to distinguish between benign and malignant activity (Figure 1).
Figure 1
PET/MRI for systemic staging of intraorbital sarcoma in a 35-year-old woman with a history of Li-Fraumeni syndrome and multiple prior malignancies, including breast and thyroid cancers. Axial T2-weighted MR (A) and fused fluorine 18–fluorodeoxyglucose (FDG) PET/MR (B) pelvic images show marked FDG activity (solid arrow) in the endometrium, which has a thickened and abnormal appearance for the patient’s age at MRI. The distinction of benign versus malignant endometrial activity at PET/CT would not be possible in this patient. Follow-up pelvic US images (not shown) showed gradually decreasing endometrial thickening, which was believed to be due to ongoing tamoxifen use. In addition, the small amount of focal FDG activity in the right ovary (open arrows) would be difficult to differentiate from a lymph node at PET/CT.
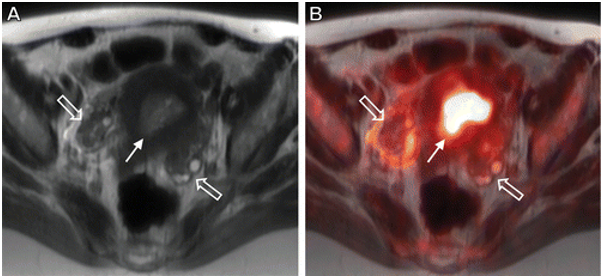
Figure 2
Initial staging 68Ga–PSMA-11 PET/MRI in a 65-year-old man with newly diagnosed Gleason 4 + 4 prostate cancer and pelvic adenopathy seen at staging prostate MRI. (A–D) Axial high–b-value diffusionweighted (A), apparent diffusion coefficient (B), T2-weighted MR (C), and fused PET/MR (D) images show a large intraprostatic tumor (arrow) occupying most of the left half of the gland. (E, F) Additional axial fused PET/MRI images show numerous subcentimeter metastatic lymph nodes (arrows) in the retroperitoneum and left supraclavicular fossa.
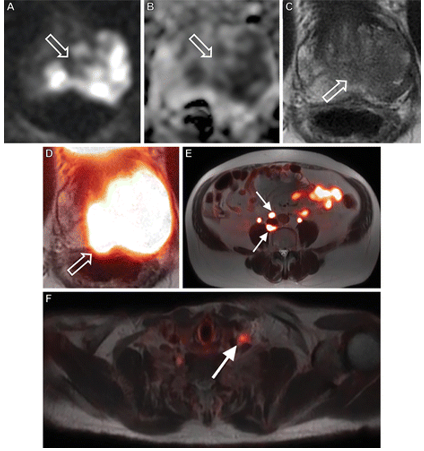
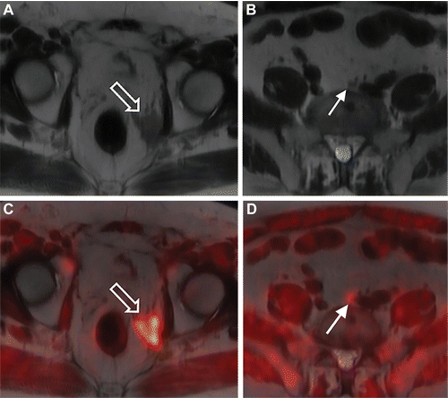
Figure 3
Fluciclovine PET/MRI in a 69-year-old man with elevated prostate-specific antigen levels (most recent, 2.1 ng/mL) who underwent prostatectomy for Gleason 4 + 3 prostate cancer 5 years earlier. Fluciclovine PET/MRI was performed to evaluate biochemical recurrence and for treatment planning. (A, B) Axial T2-weighted MR images show asymmetric T2-hypointense tissue (arrow in A) in the left prostatectomy bed and a subcentimeter left common iliac lymph node (arrow in B). (C, D) On the fused PET/ MR images, both lesions (arrow) demonstrate fluciclovine activity and are consistent with prostate cancer
The difficulties associated with interpreting PET/MRI pictures should also be known to medical professionals, since these issues can seriously impair the precision of PET/MRI data reporting. MRAC pictures may underestimate standardized uptake values for sclerotic osseous lesions due to their failure to take into account the effects of cortical bone, which could be problematic for patients suffering from sclerotic osseous metastatic disease.3 It's critical to understand the particular artifacts that can arise during PET/MRI exams in order to prevent misunderstandings. Orthopedic hardware and dental amalgam are examples of implanted metal implants that can cause dephasing on MR and MRAC images, which causes areas of PET signal loss. Examining the non-attenuation-corrected PET pictures may be helpful in certain situations.
Furthermore, while PET/MRI may allow for a more conclusive characterization of incidental lesions in comparison to PET/CT, it also results in a higher detection rate for these lesions. 4 Lastly, it has been noted that the ability of PET/MRI systems to detect pulmonary nodules and metastases may be restricted when compared to PET/CT systems (especially for nodules smaller than 10 mm), while it is unclear how this would affect patient care if these nodules are missed.5, 6, 7
Prostate Cancer
As the most prevalent noncutaneous cancer in males, prostate cancer is expected to cause 33,330 deaths and 191,930 new cases of the disease in the US in 2020. 8 According to the most recent National Comprehensive Cancer Network guidelines, patients with intermediate-, high-, or very-high-risk prostate cancer should have systemic staging using conventional imaging. This includes bone scanning with technetium 99m (99mTc) methyldiphosphonate and either CT or MRI of the pelvis and abdomen.9
Multiparametric MRI has become the go-to anatomic imaging modality for prostate cancer staging in many centers due to its greater capacity to detect intraprostatic lesions and characterize extraprostatic extension and seminal vesicle invasion. As of right now, there isn't a widely accessible and authorized PET radiotracer for the preliminary staging of high-risk prostate cancer. According to current guidelines from the National Comprehensive Cancer Network, PET/CT or PET/MRI using fluorine 18 (18F)-fluciclovine or carbon 11 (11C) choline should be used for restaging when there is a biochemical recurrence. It has been demonstrated that compared to traditional imaging alone, these investigations show more recurring illness 9, 10, 11 Due to the short half-life of 11C-choline (20 minutes) and the requirement for an on-site cyclotron, its use is restricted at many locations.
68Ga and 18F are two of the prostate-specific membrane antigen (PSMA) compounds that are being developed and studied for initial staging and biochemical recurrence assessment. Depending on the clinical situation, either a biparametric or multiparametric MRI method can be used to perform the prostate MRI evaluation. Since intraprostatic lesion detection and characterization are the most prevalent uses for the dynamic contrast-enhanced T1-weighted MRI sequence, biparametric MRI may be sufficient for initial staging when paired with whole-body PET/MRI. 12 On the other hand, dynamic contrast-enhanced magnetic resonance imaging is a crucial step in the diagnosis of recurrent prostate cancer and must to be incorporated into every instance of biochemical recurrence.
Numerous studies have assessed the use of PSMA and fluciclovine radiotracers for PET/MRI during the initial staging phase. Research on the application of fluciclovine PET/MRI 13, 14, 15, 16 has demonstrated that when compared to MRI or PET alone, PET/MRI improves the identification and characterization of high-risk prostate cancer, has a high specificity for identifying metastases to lymph nodes, and may help direct targeted biopsies. The uptake of fluciclovine in benign prostatic tissue, including benign prostatic hyperplasia, is a known drawback of the drug, limiting the PET/CT detection of malignancy in this gland. 17 Due to the enhanced ability of PET/MRI to distinguish benign prostatic hyperplasia nodules from malignant prostate lesions, this limitation may be addressed.
In a recent study, the accuracy of PSMA PET/MRI for initial staging of N1 disease was found to be 93%, while the accuracy of detecting the tumor stage was shown to be high. 18 Overall, PET/MRI allows for more accurate prostate gland lesion characterisation, thorough local-regional staging using biparametric or multiparametric MRI, and enhanced PET radiotracer detection of small-volume metastatic disease at initial staging (Figure 2).
Because fluciclovine and PSMA radiotracers provide better imaging than traditional anatomic imaging, there is substantial data to support their usage in the context of biochemical recurrence. Due to radiotracer activity in the colon and poor soft-tissue characterisation, characterization of PET activity in the pelvis (especially the prostatectomy bed, the vesicourethral anastomosis, and close to the urinary bladder) might be difficult with noncontrast PET/CT. To improve the sensitivity of disease diagnosis and precisely characterize and localize activity in the pelvis, PET/MRI allows the areas of common recurrence to be examined on PET and multiparametric MR images (Figure 3).
Both multiparametric MRI and PET/MRI are helpful in detecting recurring disease, according to researchers in a new study19 on fluciclovine PET/MRI in cases of biochemical recurrence. These scans also raised reader confidence in defining 10 out of 15 lesions with a discrepancy. Further research examining the use of PSMA PET/MRI in cases of biochemical recurrence has demonstrated that this imaging modality may be associated with a high detection rate, especially for local recurrence and patients with lower prostate-specific antigen values, and may be cost-effective by eliminating the need for multiple imaging examinations. 20, 21, 22
Conclusion
PET/MRI is being studied and employed in oncologic imaging applications more and more, despite being regarded as a relatively new imaging modality. PET/MRI provides clear advantages over PET/CT and MRI and is particularly well suited for oncologic applications in the pelvis, notably in prostate cancer, due to its superior soft-tissue characterisation and ability to obtain nearly perfect image coregistration.
It is expected that PET/MRI applications in pelvic oncology, particularly those for prostate cancer and NETs, will continue to rise given the rising usage of MRI and the ongoing discovery and licensure of radiotracers. The comfort and tolerance of the patient come first, even if PET/MRI can be a thorough imaging study. To optimize the PET and MRI data, careful planning and selection of targeted imaging techniques should be taken into account.
