- Visibility 723 Views
- Downloads 57 Downloads
- Permissions
- DOI 10.18231/j.agems.2022.018
-
CrossMark
- Citation
Asymmetric bilateral optic neuritis as the first presenting feature secondary to undiagnosed vitamin-B12 deficiency
- Author Details:
-
Anushree CM
-
Mohini Agrawal *
-
Imroz Jindal
-
Atul Bhirud
-
Byomkesh Swain
Abstract
Vitamin b12 deficiency (VBD) rarely cause involvement of optic nerve. Moreover, optic atrophy has been reported more commonly than optic neuritis secondary to VBD. Here, we report a 31-years old male presenting with bilateral but asymmetrical optic neuritis as the first clinical presentation secondary to undiagnosed VBD and showed drastic improvement in the vision after replacement with parenteral followed by oral Vitamin-B12. Thus, patients with ocular manifestations should be screened for VBD as well, particularly in the vegans. Though, VBD rarely cause optic neuritis, it should still be considered as one of the differentials; early diagnosis of which may prevent ocular morbidity.
Introduction
Vitamin B12 deficiency (VBD) seldom establishes with visual symptoms. The ophthalmologic involvement can be a first clinical feature or a neurological complication of the deficiency. Majority of the cases reported till date in the literature have described optic atrophy without optic neuritis.[1], [2], [3], [4] Optic neuritis, though rare, has been reported secondary to VBD.[1], [2], [3], [4] Like other neurological manifestations of VBD, ocular involvement is relatively less unspoken. Optic nerve damage is thought to be via degeneration.
This case report aims at describing a rare case of asymmetrical bilateral optic neuritis as the presenting feature in a young male with undiagnosed vitamin B12 deficiency.
Case Report
A 31-years-old male presented with insidious onset and gradually progressive blurring of vision in the left (OS) followed by right eye (OD) associated with mild pain on ocular movements for 25 days duration. It was associated with intermittent excruciating headache with no history of watering, redness, trauma to the eyes, or any conjunctival discharge. The patient gave no history of loss of consciousness or vomiting. Personal and family history was unremarkable.
On general physical examination patient was a well-built male, conscious and well oriented to time, place and person. His vitals were stable with unremarkable systemic examination.
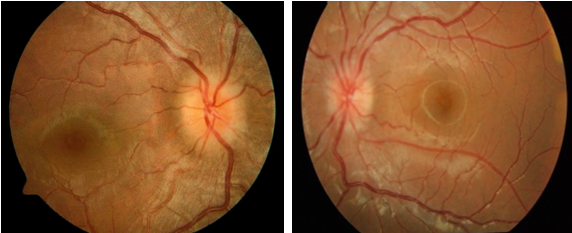
On ocular examination, his best- corrected visual acuity (BCVA) was 6/12 OD and 6/60 OS. He identified 2/16 Ishihara colour plates from each right and left eye. Pupillary examinations and extra ocular muscle movements were normal but there was mild pain in the movements of left eye. Rest anterior segment examination of both eyes was normal. On indirect ophthalmoscopy, fundus revealed mild hyperaemic disc OD and significant hyperaemic optic disc OS ([Figure 1]).
The patient was admitted as a case of severe bilateral optic neuritis and was started on with intravenous methyl-prednisolone (IVMP) for 3 days, followed by oral prednisolone. But there was no improvement in his vision. Meanwhile, detailed haematological workup was done. Complete blood count showed no abnormality. Acute phase reactants were within normal limits. Viral markers, antinuclear antibody and serum ACE were negative, thus this ruled out any possibility of vasculitis with optic nerve involvement.
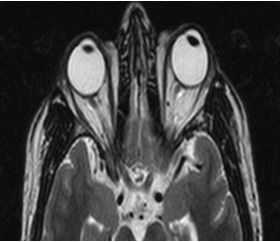
Automated visual field perimetry (OS) showed paracentral scotoma. VEP showed prolonged P100 latency in left eye. MRI orbit showed tortuosity, altered signal intensity with prominence in cerebrospinal fluid sleeve of left optic nerve ([Figure 2]).
Further, patient underwent evaluation for toxic, nutritional, genetic and autoimmune pathologies to find out the origin of optic neuropathy.
On detailed workup, he was diagnosed with optic neuritis secondary to VBD (118pg/ml); based on diagnosis of exclusion for other causes of optic neuritis, no improvement after IVMP unlike demyelinating diseases like multiple sclerosis and report of VBD with entirely normal biochemistry otherwise.
Upper GI endoscopy was done with biopsy revealing mild chronic gastritis with no H pylori. The patient was managed with intramuscular (im) cyanocobalamin (1mg/ml weekly) for 4 weeks. He showed drastic improvement in the vision in both the eyes with the replacement of Vitamin-B12.
After 4 weeks, fundus revealed resolution of optic neuritis and vision improvement with visual acuity reaching to 6/9 OD and 6/12 OS. He was directed to continue vitamin replacement with oral cyanocobalamin (1000 mcg/day).
Discussion
Vitamin B12 deficiency is, every so often, overlooked in our clinical practice. Moreover, ocular involvement is an infrequent manifestation of VBD that can be one of the presenting clinical features of the deficiency. Literature mentions about many cases with optic atrophy but without precedence by any inflammation.[1], [2], [5], [6], [7]
However, two cases have been defined earlier as optic neuritis in association with VBD.[1], [2] Like other neuropsychiatric symptoms, today’s literature on the causative metabolic pathway remains unclear.[8]
Optic neuropathy secondary to VBD occurs among <1% of B12 deficient patients,[9] amongst them, optic neuritis is very rare compared to optic atrophy. Optic atrophy courses via a more chronic as well as painless vision loss. Whereas, optic neuritis characteristically presents with acute, unilateral and painful vision loss. Reduction in color vision and central or caecocentral scotomas are present. The optic nerve, many of the times, may look normal in the early stages until optic atrophy sets in. Optic atrophy in VBD has been reported a few times in the literature, but to the best of our knowledge, optic neuritis has been reported only twice before, our case being the third such case.
Among two cases, the first case was a 47-years-old male with bilateral decrease in vision and paracentral scotoma and found to have VBD but the vitamin levels were not reported. Patient improved after im cyanocobalamin.
The second case was an 11-years-old female who presented with similar ocular complaints and was diagnosed of optic neuritis based on clinical, imaging and VEP findings. Although the VBD was not quantified, the authors mentioned a very low level upon diagnosis. However, here the patient progressed to optic atrophy and eventually ended up with complete blindness even after im cyanocobalamin administration. The ocular symptoms started two weeks before the presentation, indicating either the patient had a sub-clinical involvement or the duration of symptoms had no role in determining reversibility.
High levels of homocysteine presumably damage vascular endothelial cells via free radical generation. This could be the reason for optic neuropathy secondary to VBD.[10]
Along with typical clinical presentation, the diagnosis of optic neuropathy secondary to VBD entails thorough history, in-depth ocular examination, serum VitB12, folate, and homocysteine levels.[3]
Diagnosing VBD can be difficult based on serum B12 levels alone. Deceitfully normal levels can be seen in other disorders like liver disease and falsely low levels can be seen in folate deficiency.[10] It is helpful to measure methylmalonate and homocysteine, which are precursors in the B12 pathway, as 85% of patients with B12 deficiency will have elevated levels of these compounds.[10] This is particularly useful when the B12 level is in the low- to borderline-low range. Imaging of brain and orbits helps to rule out compressive, ischemic, inflammatory, demyelinating, or infiltrative etiologies.[11]
Prompt vitamin replacement is the mainstay of the treatment in VBD with im injections (1 mg weekly x 8 weeks followed by 1 mg monthly for life or until the underlying etiology is eradicated). One of the reports mentions better response with hydroxocobalamin (1000μg twice/week) compared to cyanocobalamin replacement concerning ocular symptoms.[12]
Early replacement of Vit B12 helps in visual recovery in the initial three months of the treatment.[11] In most of the cases reported till date, the visual symptoms either resolved entirely or did not improve or even deteriorated. Incomplete treatment of VBD with oral folic acid alone, can actually exacerbate the neurological manifestations related to VBD, if the B12 deficiency is not corrected first.
Conclusion
Patients with ocular signs and symptoms should be screened for Vitamin-B12 deficiency as well, particularly in the vegans. Though, Vit B12 deficiency rarely cause optic neuritis, it should still be considered as one of the differentials; early diagnosis of which may prevent ocular morbidity.
Source of Funding
None.
Conflict of Interest
None.
References
- Jalil A, Usmani H, Khan M, Blakely E, Taylor R, Vassallo G. Bilateral paediatric optic neuropathy precipitated by vitamin B12 deficiency and a novel mitochondrial DNA mutation.. Int Ophthalmol. 2013;33(6):687-90. [Google Scholar]
- Ellis P, Hamilton H. Retrobulbar neuritis in pernicious anemia. Am J Ophthalmol. 1959;48(1):95-7. [Google Scholar]
- Ata F, Bilal A, Javed S, Chaudhry H, Sharma R, Malik R. Optic neuropathy as a presenting feature of vitamin B-12 deficiency: A systematic review of literature and a case report. Ann Med Surg. 2020;60:316-38. [Google Scholar] [Crossref]
- Chavala S, Kosmorsky G, Lee M, Lee M. Optic neuropathy in vitamin B12 deficiency. Eur J Intern Med. 2005;16(6):447-55. [Google Scholar]
- Chu C, Scanlon P. Vitamin B12 deficiency optic neuropathy detected by asymptomatic screening. BMJ Case Rep. 2011;26. [Google Scholar] [Crossref]
- Foulds W, Chisholm I, Stewart J, Wilson T. The optic neuropathy of pernicious anemia. Arch Ophthalmol. 1969;82(4):427-59. [Google Scholar]
- Dobson R, Alvares D. The difficulties with vitamin B12. Pract Neurol. 2016;16(4):308-19. [Google Scholar]
- Lachner C, Steinle N, Regenold W. The neuropsychiatry of vitamin B12 deficiency in elderly patients. J Neuropsychiatry Clin Neurosci. 2012;24(1):5-15. [Google Scholar]
- Lennihan L, Rowland L. Nutritional disorders: malnutrition, malabsorption, and B12 and other vitamin deficiency. Merritt’s Neurol. 2010. [Google Scholar]
- Pianka P, Almog Y, Man O, Goldstein M, Sela B, Loewenstein A. Hyperhomocystinemia in patients with nonarteritic anterior ischemic optic neuropathy, central retinal artery occlusion, and central retinal vein occlusion. Ophthalmology. 2000;107(8):1588-92. [Google Scholar]
- Chan J. . Compressive and infiltrative optic neuropathies. InOptic Nerve Disorders. 2007. [Google Scholar]
- Toosy A, Mason D, Miller D. Optic neuritis. Lancet Neurol. 2014;13(1):83-99. [Google Scholar]
How to Cite This Article
Vancouver
CM A, Agrawal M, Jindal I, Bhirud A, Swain B. Asymmetric bilateral optic neuritis as the first presenting feature secondary to undiagnosed vitamin-B12 deficiency [Internet]. Ann Geriatr Educ Med Sci. 2022 [cited 2025 Oct 14];9(2):88-90. Available from: https://doi.org/10.18231/j.agems.2022.018
APA
CM, A., Agrawal, M., Jindal, I., Bhirud, A., Swain, B. (2022). Asymmetric bilateral optic neuritis as the first presenting feature secondary to undiagnosed vitamin-B12 deficiency. Ann Geriatr Educ Med Sci, 9(2), 88-90. https://doi.org/10.18231/j.agems.2022.018
MLA
CM, Anushree, Agrawal, Mohini, Jindal, Imroz, Bhirud, Atul, Swain, Byomkesh. "Asymmetric bilateral optic neuritis as the first presenting feature secondary to undiagnosed vitamin-B12 deficiency." Ann Geriatr Educ Med Sci, vol. 9, no. 2, 2022, pp. 88-90. https://doi.org/10.18231/j.agems.2022.018
Chicago
CM, A., Agrawal, M., Jindal, I., Bhirud, A., Swain, B.. "Asymmetric bilateral optic neuritis as the first presenting feature secondary to undiagnosed vitamin-B12 deficiency." Ann Geriatr Educ Med Sci 9, no. 2 (2022): 88-90. https://doi.org/10.18231/j.agems.2022.018
