Introduction
The World Health Organization (WHO) estimates that globally three million intentional or un-intentional pesticide poisoning episodes occur annually and out of these a minimum of three lakhs die.1 It seems these data represent only the tip of iceberg, as most cases are not reported from developing nations. Organophosphorus insecticides are arguably one of the commonest causes of morbidity and mortality due to poisoning worldwide, especially in developing countries like India. Causes of poisoning are suicidal, accidental and homicidal. Suicidal poisoning is the most common cause in developing countries because of cheap and easy availability in market. Their ease of access and socio cultural factors play important role in choice of OP compound as self-poison.2
The morbidity and mortality outcome depends on the time lag between exposure and the onset of management. Therefore, it is cardinal to recognize the entire spectrum of the symptoms. Organophosphorus (OP) compounds inhibit acetyl cholinesterase and butyryl cholinesterase enzymes resulting in over stimulation at cholinergic synapses.3 Symptoms are classified into muscarinic, nicotinic and central depending on the actions over the respective receptors. Muscarinic features include excessive salivation, lacrimation, urination, diarrhoea, gastrointestinal cramps, emesis, blurred vision, miosis, bradycardia, and wheezing. Nicotinic features include fasciculation, paresis or paralysis, hypertension and tachycardia. Three types of neuro muscular paralysis are noticed. Type I is due to continued depolarization at neuro-muscular junction, type II due to intermediate syndrome and type III due to delayed polyneuropathy. Central features include anxiety, confusion, seizures, psychosis and ataxia.4
Laboratory evidence of OP poisoning is usually confirmed by measuring the decreases in the BChE and EChE activities. However, because of wide inter-individual variability, significant depression of the enzyme cholinesterase activity may occur but still fall within the "normal" range. Also, estimation of either serum EChE or BChE levels is costly and not regularly performed in most laboratories.5 There are emerging options for new cheaper and/or easily quantifiable biochemical markers in relation to OP poisoning like creatine phosphokinase (CPK), lactate dehydrogenase (LDH) and serum immunoglobulins (IgG, IgA). But immunoglobulin assays, apart from being costly and difficult to perform in most laboratories, are often unreliable.6 Several animal model studies proposed that serum level of CPK is often found to be elevated in OP poisoning, and it may be used as a biomarker.7 Therefore, this study was conducted to assess the correlation between serum CPK levels and the severity of acute OP poisoning.
Material and Methods
The present study was carried out in a tertiary care hospital in southern India. Patients admitted to hospital less than 24 hrs with of history of OP poisoning were included in the study. Patients with pre-existing myopathy, epilepsy, myocardial infarction, myocarditis chronic renal disease and trauma were excluded from the study. Presumptive diagnosis of organophosphorus poisoning was based on history, circumstantial evidence and characteristic clinical features. Gastric lavage contents were sent for analysis to poison detection centre. Clinical severity was categorized according to Peradeniya organophosphorus poisoning (POP) scale, (0–3, Mild Poisoning; 4–7, Moderate Poisoning; 8–11, Severe Poisoning) as shown in (Table 1).8 The ethical committee approved this study.
Table 1
Peradeniya Organophosphorus poisoning (POP) severity scale
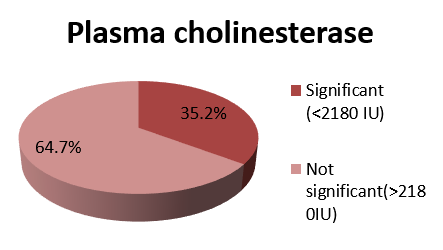
Blood samples for serum CPK total and plasma cholinesterase were collected at time of admission. Other investigations done were random blood glucose estimation of serum electrolytes (Sodium and Potassium), blood urea and serum creatinine, complete blood picture, chest radiograph, electrocardiogram, HIV, HBsAg, liver function test and ABG (if necessary). The data was analyzed and computed. Normal values of CPK and serum cholinesterase are 15-125 U/L and 2180-9180 U/L.
Results
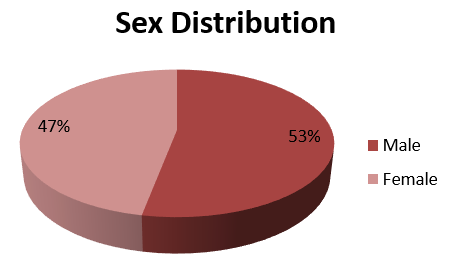
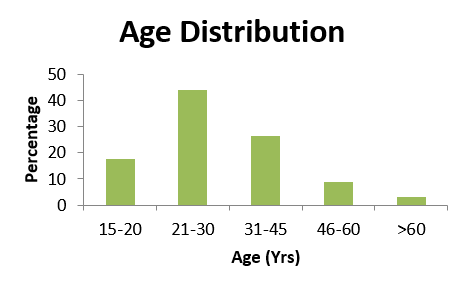
Out of thirty-four patients enrolled in the study, 18 (53.0%) were males and 16 (47.0%) were females (Figure 1). They were aged from 16 to 90 years. Most common age group was 21-30 years (44.1%) (Figure 2).
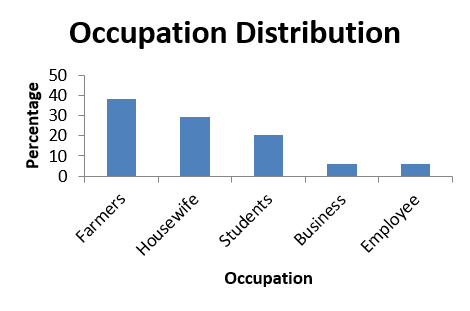
Nineteen patients (55.8%) came from rural areas, whereas 15 (44.2%) from urban areas. Regarding occupation, 13 (38.2%) were farmers, 10 (29.4%) housewives, 7 (20.5%) students (Figure 3). The most common route of exposure was oral (85.2%), the most common manner of poisoning was suicidal manner (88.9%). Most common OP compound was Monocrotophos (46.0%).
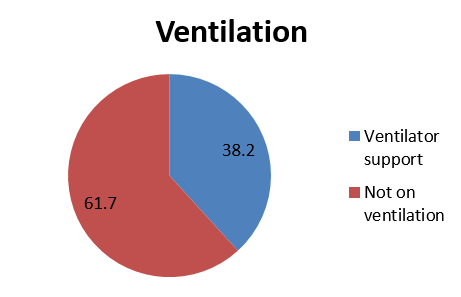
Out of thirty four patients, 13 (38.2%) patients required ventilator support (Figure 4), plasma cholinesterase was significantly reduced in 35.2% patients, (Figure 5) and creatine phosphokinase was significantly raised in 41.4% patients (Figure 6).
Discussion
In this study male: female ratio is 1.1: 1. There was male preponderance. A study conducted by Gupta SK et al. in 413 patients found 273 patients were male. Male: female ratio is 1.9:1.9 Incidence of organophosphorus poisoning was more among the age group 21-30 years (44.1%). This is the most critical period, when one is likely to face various problems that may lead to psychological stress, so a person may take drastic steps to end his life by consuming available poisons. Similar results were seen in studies conducted by Gupta SK et al.9 Dayanand Raddi et al. 2 and Hundekari IA et al.10 A study conducted by Gupta SK et al. out of 413 patients, 139 patients were in the age group of 21-30 years. A study conducted by Dayanand Raddi et al. out of 320 patients, 144 patients were in the age group of 21-30 years. A study conducted by Hundekari IA et al. out of 92 patients, 58 patients were in the age group of 15-25 years.
The most commonly used OP compounds were monocrotophos (46.0%), chlorpyrifos (15.0%). Monocrotophos is commonly used pesticide in the paddy fields and it’s easily available in the market. Monocrotophos (30.17%) was most common compound in a study conducted by Gupta SK et al. then followed by methyl parathion (28.44%) and quinolphos (18.96%).9
In this study, it was found that maximum cases were suicidal poisoning 30 (88.9%). It might may be due to rapid urbanization, social and economic factors which mainly contribute to frustration and depression in the people. The persons who are not able to cope up the stressful situations are the major victims of suicidal poisoning. Choice of OP compound for suicide is mainly due to cheap and easy availability. Similar result was seen in a studies conducted by Dayanand Raddi et al. (97.5%).2, Hundekari IA et al. (95.3).10 Kar SM et al. (95.2%). 11 Studies conducted by Dayanand Raddi et al., out of 320 patients, suicidal patients were 312 (97.5%). A study conducted by Hundekari IA et al. out of 150 patients, 143 (95.3%) patients was suicidal. Studies conducted by Kar SM et al. out of 65 patients, 64 patients were suicidal.
In this study, most of the patients were farmers (38.2%), housewives (29.4%) and students (20.5%). Farmers are more prone for OP poisoning; it might be due to easy availability and accessibility of the pesticides among them. Among the symptoms, vomiting was most common symptom. Out of 34 patients, 30 (88.9%) patients had vomiting, followed by miosis (82.5%), sweating (72%), bradycardia (70%), and salivation (52%). Vomiting is most common symptom because of the practice of induced emesis by giving salt water in this area because of lack of knowledge.
Out of thirty-four patients, 13 (38.2%) were severe according to POP scale. More severity of poisoning according to POP scale, patient required ventilator support and prolong hospital stay. Total dose of atropine and PAM requirement also increased. Total 13 patients required ventilator support, out of them six had monocrotophos poisoning and three had chlorpyrifos poisoning requiring ventilator support.
Plasma cholinesterase inhibition is correlating well with clinical severity in case of OP poisoning. Our findings reduction of plasma cholinesterase on day of admission and severity of OP poisoning are consistent with Wadia et al. who showed good correlation between plasma cholinesterase level and severity of poisoning. Plasma cholinesterase showed a trend of increase in activity with treatment of atropine and pralidoxime during the course of hospital stay.4
This study showed that as the POP scale increases serum CPK levels increase; meanwhile plasma cholinesterase levels decrease. These findings were statistically highly significant (p <0.001). There was a high degree of correlation between the initial serum CPK level and the severity of acute OP poisoning; i.e. positive correlation with (POP scale and total dose of atropine "mg" and obidoxime "g") and the negative correlation with (Plasma cholinesterase). These correlations were found to be statistically highly significant (P < 0.001).
Study conducted by Bhattacharya et al. who confirmed the presence of a high degree of correlation between initial CPK value and POP scale, serum EChE levels, arterial pH values and total dose of atropine in acute OP poisoning. Muscle fiber necrosis and consequently raised CPK levels occur in severely acute OP poisoned patients. So, cheaper, easily quantifiable and more available biochemical markers in relation to OP poisoning like serum CPK can be used in predicting as well as assessing the prognosis of patients with OP poisoning.6
Three types of muscle injuries (paralysis) are noticed in OP poisoning. Type I is due to continued depolarization at neuro-muscular junction, type II due to intermediate syndrome and type III due to delayed polyneuropathy.4 In this study, the elevated serum CPK levels were confirmed during the acute stage of toxicity i.e. all cases presented within 24 hours of exposure to OP compounds and before the development of the intermediate syndrome. Intermediate syndrome occurs in between the periods of acute and delayed OP toxicity. Intermediate syndrome occurs in patients 24–96 hours after acute OP poisoning. Raised CPK levels occur due to rhabdomyolysis in ― intermediate syndrome.12
Study conducted by Sahjian and Frakes stated that if there is ongoing injury to the muscle due to development of complications, the CPK level continues to be elevated, since half-life of CPK is about 1.5 days; it normalizes within 5–6 days of a single insult to the muscle.13 Study conducted by Perreault et al. confirmed that when a skeletal muscle is injured, CPK leaks into the blood and urine. Serum CPK level remains the best biomarker for detecting and monitoring skeletal muscle damage and diseases.14 Some studies confirmed that elevation of serum CPK levels in acute OP poisoning, especially if the patient is severely poisoned, presumably due to muscle fiber necrosis. However, the main disadvantage of serum CPK as a biomarker for acute OP poisoning, its non-specificity. So exclusion of other conditions and diseases that may cause its elevation in patients with acute OP poisoning is mandatory.