Introduction
This case report depicts the unusual presentation of a 60 years old male who presented with subcutaneous emphysema, hoarseness of voice and dysphagia all due to squamous cell carcinoma of supraglottic larynx with local metastasis. In general, the term subcutaneous emphysema is associated with internal or external trauma. Here, we are depicting a rare case as in where the tumour growth from within the laryngeal cartilage caused the perforation of the cartilage leading to a channel of connection between airway and subcutaneous plane of neck leading to subcutaneous emphysema. The case also shows how the local extension of a tumour can present in a variety of manner before the definitive symptoms appear and that it can be difficult to diagnosis the root cause of such presentation.
Case Report
A 60 years old male presented in emergency department with complaints of hoarseness of voice insidious in onset for 3 years, difficulty and pain while swallowing food for 3 months and swelling around the neck till the anterior part of chest associated with breathlessness in the last 2 weeks. There was no history of recent trauma around the neck, previous history of intubation or tracheostomy or any past history suggestive of chronic lung disease. He consumed around 100 ml of alcohol per week for the last 20 years and bidi smoker for last 10 years. On taking a detailed account of his condition, it was revealed that he also had history of weight loss of about 15 kgs in the last six months, and he also revealed about decreased appetite in the last 1 year.
On general examination patient was conscious, oriented and showed respiratory distress with a respiratory rate of 30 cycles per minute. His blood pressure was 140/90 mmhg with a pulse rate of 106/min and his oxygen saturation was 92% on room air. On systemic examination, his respiratory system showed prominence of accessory muscles of respiration, chest wall was showing a swelling a swelling on its anterior surface which was extending from around the neck. On percussion and auscultation on lung fields, there was no significant finding and air entry was equal bilaterally. Central nervous system examination was a normal study with intact sensorium. On per abdomen examination, there were no signs of tender or organomegaly and normal peristaltic sounds were heard. Cardiovascular system examination was s/o normal heart sounds and no other significant anomaly. His routine blood investigations were within normal limits with Hb- 15.3 gm%, WBC-6600 cells per cubic mm, PLT-1.73 lacs per cubic mm, MCV-92.5 fL, serum urea-62 mg/dl, creatinine-1.2 mg/dl, Na-148 meq/dl, K-3.5 meq/dl, serum LDH-221, HBA1C-6.7, ALP-121 IU/L,SGPT-28 IU/L, SGOT-65 IU/L, total bilirubin-1.0 mg/dl, conjugated bilirubin-0.3 mg/dl, unconjugated bilirubin-0.7 mg/dl, RBS-106 mg/d.
On local examination, the swelling extended from left side of the left post auricular region to around the neck and then onto anterior chest wall. There was an ulcer present over the neck which showed a local site hematoma. On palpation, the swelling was soft to touch and crepitations could be heard upon applying pressure. It was not associated with pain or tenderness. There was no evidence of any trauma or any excoriation marks over the swelling. Computed tomography of neck was s/o ill-defined heterogenous iso-dense to hypodense thickening involving left aryepiglottic, posterior hypopharyngeal wall, bilateral true and false vocal cords, cricoid and thyroid cartilage altogether leading to considerable cervical compromise. It also suggested of an ill-defined polypoidal lesion (1.8 x 1.6 cm) prominently involving the right true and false vocal cord which was seen compromising the airway. Surgical emphysema was noted on the left side of the neck extending to the anterior chest wall. There were few enlarged lymph nodes in the right submandibular region with the largest measuring 14 mm.
Patient was planned for fine needle aspiration cytology from right submandibular lymph node under guidance of ultrasonography. During USG neck, the largest lymph node was round, hypo-echoic with presence of micro-calcifications suggestive of malignant lymph node involvement. Slides were prepared and the sample was sent for detailed microscopic examination. Figure 2 is the image captured during FNAC of the lymph node.
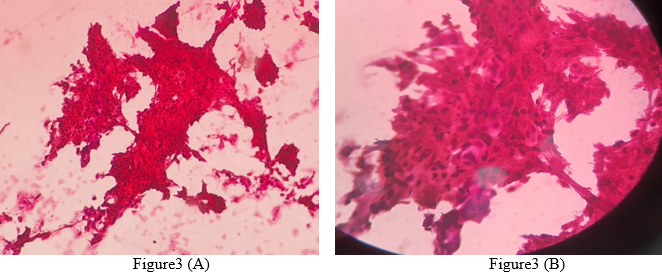
The histopathology report was suggestive of small sheets of squamous cells with hyperchromatic, mildly pleomorphic, angular, spindle nuclei. Background showed cytoplasmic flakes, macrophages and few leucocytes along with haemorrhagic materials. The entire findings were suggestive of well differentiated squamous cell carcinoma. The following 2 Figure 3(A) and (B) show the findings durin
microscopy.
Discussion
When air is injected into the fascial planes of the connective tissue through a trauma site, subcutaneous emphysema develops.1 Neck subcutaneous emphysema is an uncommon condition caused primarily by iatrogenic and traumatic causes.2 Air is generally found in the nose, paranasal sinuses, mouth, pharynx, larynx, and trachea in the head and neck. It can be present in the thorax's airways, alveoli, and oesophagus. Air should only be present in hollow viscera in the belly, such as the stomach, small bowel, and colon. The presence of gas in the pulmonary interstitium, subcutaneous tissue, mediastinum, and soft tissues of the neck or retroperitoneum indicates a pathogenic process that should be investigated.3 The insertion of air under pressure under the fascial gaps of tis.sue is the underlying pathophysiological mechanism. As a result, the very thin connective tissue between adjacent muscle planes is dissected.2 Three pathologic situations may give rise to soft-tissue cervical emphysema clinically:
It can be due gas producing bacteria like clostridia which can be present due to any local infection;
It can be due to perforation of mucosal linings of the airway or GIT leading to leakage of air from within; and
It can arise spontaneously whenever the alveoli rupture due difference in the pressure gradient between the alveoli and the surrounding structures,3
Air-containing structures such as the paranasal sinuses, oropharynx, proximal airways, and digestive system hollow viscera are all potential sources of soft-tissue emphysema after trauma.3 Mucosal or skin flaps operate as one-way valves, and the suction force for air to be sucked in is most likely negative pressure in the subcutaneous tissue. The trapped air in the head and neck is frequently limited to the subcutaneous area. It can, however, disseminate profoundly along the neck's fascial planes, resulting in para- and retropharyngeal emphysema, with probable extension into the thorax and mediastinum.1 In the diagnosis of subcutaneous emphysema, computed tomography (CT) has become the gold standard. These tests can be done with or without the use of a contrast media. Contrast may help distinguish between loculations like active infection and radiolucencies like subcutaneous emphysema.4 Subcutaneous emphysema can produce chest wall compression, leading to respiratory and hemodynamic stress.5, 6, 7, 8, 9 Although the treatment is cautious, most doctors recommend delivering 100 percent oxygen to speed up gas resorption. Antibiotic prophylaxis may help to prevent mediastinitis and abscesses in the neck. In uncomplicated cases, emphysema will resolve on its own in 1-2 weeks.1
A similar case report has been reported by Pezier et al. in 2014 whereby an 82 years old male presented with subcutaneous emphysema due to malignancy of larynx.10
Conclusion
Assessment of emphysema therefore should be carried out in a step-wise manner and once its pathophysiology is understood, accordingly causes should be ruled out. Not to forget the fact that trauma not necessarily means blunts force trauma or trauma during intubation or any other surgical pressure, it can also suggest an intra-luminal compressing mass like in our case which can eventually lead to internal rupture than subsequent emphysema. This being cleared, the primary line of management will always be emergency protocol of airway-breathing-circulation-disability-exposure.11