Introduction
Osteoarthritis is the most commonly encountered disease of the musculoskeletal system and it is the major cause of disability and socioeconomic burden.1
Osteoarthritis is a chronic degenerative disorder of multifactorial etiology, including acute and/or chronic insults from normal wear and tear, age, obesity and joint injury.2 OA is characterized by degradation of the articular cartilage, resulting in an alteration of its biomechanical properties.3 This contributes to focal loss of articular cartilage, loss of joint space, osteophytes formation, focal areas of synovitis, periarticular bone remodeling and subchondral cysts.4
Symptomatically, the most commonly affected joint in OA is the knee joint.5 At the knee joint soft tissue changes can include decrease in the strength of the quadriceps and sagittal range of motion, as well as increased soft tissue contracture. Collectively these changes produce the typical clinical picture of joint pain; worsening symptoms with activity and weight bearing and stiffness developing at rest. These facilitate the decline in physical function and progression of the disability.4
There is higher prevalence of OA with advanced age and in females.6 In fact, most knee pain in the elderly is due to OA.7 Knee OA produces significant changes in health-related quality of life, particularly physical, mental and social components of health.
Figures regarding prevalence of symptomatic knee OA in the general population vary, with estimates of 7.2% in those aged 40 or older, 12.5% in those aged over 45 and 14.8% in those aged 50 or older.8, 9
The treatment of knee OA is currently limited to the management of symptoms rather than reducing disease progression. Common current treatment strategies involve pharmacological treatments, non-pharmacological treatments and surgical interventions.10
Whilst these forms of therapy held to deal with symptoms, OA is often viewed as a problem of biomechanical function. To address the concerns of lost function, including the ability to ambulate, several forms of physical therapy have been advocated, with various strength based and exercise programs the cornerstone of treatment. Prescription of an aerobic walking and quadriceps strengthening program had been used successfully, producing a reduction in both pain and disability.11
Multimodal approaches utilizing a combination of exercises and individualized manual therapy has resulted in significant improvements in knee pain and function when compared to a placebo therapy of sub therapeutic ultrasound in both the short term and long term follow-up.12 Individualized manual therapy and a home exercise program was compared over a 4 week period to a home exercise program and resulted in decreased knee pain and improved function in the short and long term.13
A number of mechanisms have been proposed to explain how the hypoalgesic effects of passive joint mobilization may be mediated. Local mechanical disturbance may modify the clinical environment and thereby alter the concentration of inflammatory mediators.14 Movement may also trigger segmental inhibitory mechanisms.15 In addition it has been hypothesized that mobilization may activate descending pain inhibitory systems, mediated supraspinally.16 Human studies have demonstrated that joint mobilization produces rapid hypoalgesia with concurrent sympathetic nervous system and motor system excitation.17 Therefore use of manual therapy should be offered as an alternative to pharmaceutical administrations.
A literature synthesis revealed that there is a level of B or fair evidence for manipulative therapy of knee combined with multimodal or exercise therapy for knee osteoarthritis and concluded that additional, larger and methodologically improved studies are needed and merited.18, 19 Manual therapy treatment for knee arthritis was concentrated on the arthrokinematic movements which give good pain relief .
Thus the purpose of this study is to compare the effectiveness of Maitland mobilization and the conservative protocol on the pain and the functional mobility of patients with OA of knee joint.
Aims and Objectives of the Study
To find out the effect of Maitland’s mobilization on improvement in pain and functional mobility of the patients with osteoarthritis of knee joint.
To compare the effect of conservative Rx and Maitland’s mobilization on pain and functional mobility of the patients with osteoarthritis of knee joint.
Hypothesis
Experimental hypothesis
There will be significant improvement in pain and functional mobility following the Maitland’s mobilization techniques as compared to control group in patients with OA knee.
There will be significant difference between conservative Rx and Maitland’s mobilization in reducing pain and improving functional mobility of patients with OA knee.
Null hypothesis
There will be no significant improvement in pain and functional mobility following the Maitland’s mobilization techniques as compared to control group in patients with OA knee
There will be no significant difference between Maitland and conservative Rx techniques over the control group in reducing pain and improving functional mobility of patients with OA knee.
Review of Literature
Fleetwood-Walker SM et al. (2007) Heat has been used therapeutically for thousands of years.20 It offers immediate. Fleetwood-Walker SM pain relief and can increase circulation to speed the healing process after injury.21, 22, 23 For this reason, it is popular for use on many types of pain including joint and muscle pain as well as soft tissue damage.
Da-hon Lin et al. (2008) studied the effects of high resistance exercises and low resistance exercises with no exercise group on patients with knee osteoarthritis and concluded that both high and low resistance strength training improved clinical effects in terms of pain, function, walking time and muscle torque.24
R Serror et al. (2008) conducted a study to validate individualized forms of WOMAC function and subscale they found that the WOMAC top 5 was the most responsive scale and thus concluded that WOMAC top 5 could be one interesting tool in therapeutic evaluation of hip/knee Osteoarthritis.
Penny et al. (2006) studied the initial effects of accessory knee joint mobilization, comprising of a 9 minutes non noxious AP mobilization of the tibiofemoral joint, on measures of pain and function in individuals with knee osteoarthritis and concluded that accessory mobilization of an osteoarthritic knee joint produces both local and widespread hypoalgesic effects.25
Deyle et al. (2005) conducted a study to compare a home based physical therapy program comprising of conservative treatment with a clinically based physical therapy program comprising of conservative treatment along with manual therapy and concluded that subjects in the clinic treatment group achieved about twice as much improvement in WOMAC scores than the subjects who were in the home exercise group.13
Michael D. Lewek et al. (2004) studied the extent of quadriceps muscle weakness and activation failure in middle-aged patients with symptomatic medial knee osteoarthritis using maximum voluntary isometric contractions (MVIC) and a burst superimposition technique and concluded that subjects with knee OA had significantly less quadriceps strength relative to body mass index (BMI).26
Sambajon VV et al. (2003) conducted a study to examine the effect of mechanical strain on synovial fibroblasts production of inflammatory prostaglandins E(2) (PGE(2)) and protineases in patients with arthritic diseases and concluded that continuous passive motion as in mobilization reduces the PGE(2) production in synovial fibroblasts and thus decreases inflammatory mediators.
Mao-Huang et al.(2003) compared effects of various therapeutic exercise on the functional status of patients with knee osteoarthritis and concluded that is kinetic, isotonic and isometric muscle strengthening exercises had significant effect on pain reduction, disability reduction, and in walking speed after treatment and at follow-up when compared with their initial status.
Lucie Brosseau et al. (2003) conducted a study to determine the effectiveness of thermotherapy in the treatment of OA of the knee and concluded that ice massage compared to control had a statistically beneficial effect on ROM, function and knee strength.
Crossley et al. (2002) conducted a study to find the efficacy of non-operative management of patellofemoral pain which comprised of quadriceps muscle retraining, patellofemoral joint mobilization, patellar taping and daily home exercises and compared this with the placebo treatment of sham ultrasound, light application of a nontherapeutic gel and placebo taping, they concluded that the physical therapy regimen is efficacious for alleviation of patellofemoral pain.27
Angst et al. (2001) conducted a study to compare the responsiveness of the condition specific Western Ontario and McMaster universities Osteoarthritis index (WOMAC) and the generic form-36 (SF-36) in patients with OA of legs undergoing a comprehensive inpatient rehabilitation intervention and concluded that both the instruments, WOMAC and the SF-36, capture improvement in pain in patients undergoing comprehensive impatient rehabilitation intervention. Functional improvements can be detected better by WOMAC than by SF-36.
Roody et al. (2001) conducted a study to assess the efficacy of aerobic walking and home based quadriceps strengthening exercises in reducing pain and disability in knee OA and concluded that both aerobic walking and home based quadriceps strengthening exercise are effective when an indirect comparison is made.22
Deyle et al. (2000) studied the effect of manual therapy applied to knee as well as to lumbar spine, hip and ankle as required and performed a standardized exercise program in the clinic and at home for the patients with knee osteoarthritis which was compared with the placebo group which received sub therapeutic ultrasound to the knee and concluded that patients in the treatment group had statistically significant gains over baseline WOMAC scores and walking distance as compared with the placebo group.12
Rowlands et al.(1999) conducted a study to investigate the efficacy of chiropractic patella mobilization in the treatment of PFPS, group A received patella mobilization and group B received detuned ultrasound as placebo, the authors concluded that there results support the potential efficacy of chiropractic mobilization for PFPS patients and suggest that patellar mobilization may be useful when combined with patient-specific treatment options such as exercise, orthoses and activity modification.28
M. V. Hurley et al. (1998) compared quadriceps sensorimotor function and disability in 60 knee OA patients, before and after an exercise regime and concluded that exercise improved quadriceps sensorimotor dysfunction and disability in the management of knee OA.
Bellamy et al. (1998) have validated The Western Onatario and McMaster Universities (WOMAC) index for specific measurements of OA patients in clinical trials.
Michael V Hurley et al. (1997) conducted a study to asses quadriceps strength,and voluntary activation in patients with knee OA and concluded that arthrogenic impairment in quadriceps sensorimotor function and decreased postural stability was associated with reduced functional performance of the patients.
Edwin E. Bunton et al. (1993) did a study on the role of limb torque muscle action and proprioception during closed kinematic chain rehabilitation of the lower extremity and conclude that closed kinematic chain rehabilitation is an economical, efficient, and effective means of rehabilitation, thus gaining lower extremity joint stability.
Materials and Methods
Method of collection of data
Total subjects in study were 30.
A consent form was given to the patient containing information regarding pre-participation data like:
Age
Sex
Site of pain
Duration
Cause
Employment status
Medical conditions
Medications
Surgery performed
To fulfill the inclusion criteria.
On the day 1 the outcome measures such as, WOMAC score,29, 30 and the VAS score was taken for all the subjects. The treatment was given thrice a week and the intervention was of 4 weeks. After 1st, 2nd, 3rd and 4th weeks the outcomes measures was reassessed.
The group 1 was given only conservative treatment, 13, comprising of
Strengthening exercises
Isometric quadriceps: Hold each contraction for 6 sec. with a 10 sec. rest in between, 10 repetitions, perform daily.
Standing terminal knee extension with resistive band or a weight cuff: Perform 3 times a week, hold each contraction for 3 sec.,10 repetitions.
Seated leg press holding a resistive band in both hands: Hold each contraction for 3 sec. 10 repetitions, progress to bands with increasing resistance.
Partial squats with arm support as needed: Hold each contraction for 3 sec.10 repetitions, progress to full body weight without support and additional bouts.
Step ups: Slowly repeat for 30 sec. progress to increased height of step and additional bouts.
The group 2 was given
Conservative treatment + Maitland’s mobilization
Mobilization grades 1 and 2 was given for pain and grades 3 and 4 was given to increase the range of motion, 2-6 bouts of 30sec. Per manual technique was given.
Mobilization was given for four weeks (thrice in a week
Glide given was Anteroposterior to the knee joint
The treatment for both the groups was given under supervision
Data recording and tabulation
The values of all the parameters of the sessions were recorded accurately in the printed data collection sheet.
The values of pre-treatment were recorded at the day-1 of the 1st week and the values of post- treatment were recorded at the end of 4th week in data sheet. The collected data were arranged under the categories of group-1 and group-2. Each group data were tabulated under sub-categories of pretreatment and post-treatment groups.
Means of these sub-category values in each group were considered for intra group analysis
Means of the difference of the scores between the sub-categories were consider for inter group analysis.
Statistical analysis
Descriptive statistics was used to calculate the mean, Standard deviation and standard error for the purpose of summarizing the data and for further analysis for the difference between the groups.
Paired samples t test was used to compare the within group effectiveness between the pre-test and the post-test measurements of VAS Score and WOMAC Score in both the groups.
The p level was kept as 0.05 and less than that level was considered as significant.
Result
Table 1
Intra group comparison of pain and WOMAC score in control group
|
Sl. No. |
Parameter |
Pretreatment |
Postreatment |
T value |
P value |
||
|
|
|
MeanE |
S.D |
Mean |
S.D |
|
|
|
1. |
PAIN |
7.13 |
1.46 |
4.93 |
1.22 |
11.00 |
0.000** |
|
2. |
WOMAC |
67.00 |
12.45 |
52.66 |
12.78 |
14.79 |
0.000** |
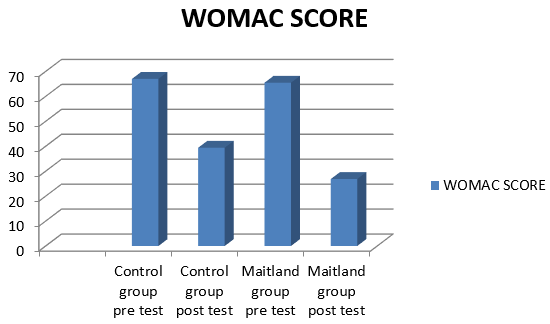
Table 1 Shows the intra group comparison of pain and WOMAC Score in control group. The mean pain score for pre and post treatment were 7.13 ± 1.46, 4.93 ± 1.22 respectively, while the mean WOMAC score for the pre and post treatment were 67.00 ± 12.45, 52.66 ± 12.78 respectively. Highly significant (p<0.001) difference was found between pre and post treatment level of pain and WOMAC Score in the control group with the t value 11.00 and14.79 respectively.
Table 2
Intra group comparisons of pain and WOMAC Score in experimental group (Maitland’s group)
|
Sl. No. |
Parameter |
Pretreatment |
Postreatment |
T value |
P value |
||
|
|
|
Mean |
S.D |
Mean |
S.D |
|
|
|
1. |
Pain |
7.27 |
1.16 |
3.53 |
0.64 |
16.36 |
0.000** |
|
2. |
Womac |
65.47 |
11.15 |
26.87 |
5.45 |
18.59 |
0.000** |
Table 2 Shows the intra group comparison of pain and WOMAC Score in control group. The mean pain score for pre and post treatment were 7.27 ± 1.16,3.53 ± 0.64 respectively, while the mean WOMAC score for the pre and post treatment were 65.47 ± 11.15, 26.87 ± 5.45 respectively. Highly significant (p<0.001) difference was found between pre and post treatment level of pain and WOMAC Score in the control group with the t value 16.36 and18.59 respectively.
Table 3
Inter group comparison of effect on VAS score and WOMAC score.
|
Sl. No. |
Parameter |
Control |
Maitland |
F value |
P value |
||
|
|
|
Mean |
S.D |
Mean |
S.D |
|
|
|
1. |
Vas |
2.13 |
0.74 |
3.73 |
0.88 |
14.2 |
0.000** |
|
2. |
Womac |
14.33 |
3.75 |
38.60 |
8.04 |
71.6 |
0.000** |
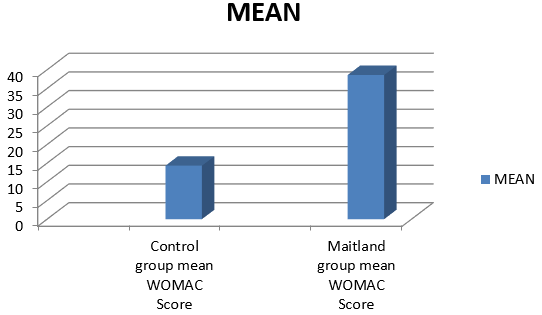
Table 3 Shows inter group comparison of effect on VAS score and WOMAC score in the control and Maitland group. For the control group the mean VAS score is 2.13± 0.74 and the WOMAC score is 14.33± 3.75. For the Maitland group the mean VAS score is 3.73± 0.88 and the WOMAC score is 38.60± 8.04. The mean values for the VAS score and WOMAC scores in two groups were significant.
Table 4
Intergroup pair wise comparison of effect on pain score.
|
Sl. No. |
Group |
Mean difference |
S.e |
95% c.i. |
P-Level |
|
|
|
|
|
|
Lower Bound |
Upper Bound |
|
|
1. |
Maitland Vs Control |
1.60 |
0.300 |
-2.33 |
-0.87 |
0.000** |
Table 4 Shows Inter group pair wise comparison of effect on pain score. The mean difference for pain between the Maitland group and control group is 1.60 which is highly significant.
Table 5
Intergroup pair wise comparison of effect on WOMAC score.
|
Sl. No. |
Group |
Mean difference |
S.e |
95% c.i. |
P-Level |
|
|
|
|
|
|
Lower Bound |
Upper Bound |
|
|
1. |
Maitland Vs Control |
24.26 |
2.03 |
-29.19 |
-19.34 |
0.000** |
Table 5 Shows Inter group pair wise comparison of effect on WOMAC score. The mean difference for pain between the Maitland group and control group is 24.26 which is highly significant.
Figure 1
The comparison of pre and post intervention mean pain in control group and Maitland’s group.
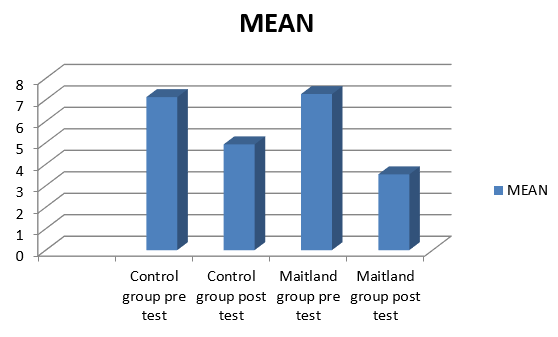
Figure 2 Shows the bar chart representation for comparison of pain in control and Maitland group at the pre (at pre-week 1) and Post (at the end of 4th week) intervention.
Figure 4 Shows the bar chart representation for the inter group comparison of VAS score.
Table 4 Shows the bar chart representation for the inter group comparison of WOMAC score.
Discussion
Osteoarthritis is a degenerative disorder which mainly affects the articular cartilage. Due to the wear and tear the cartilage undergoes micro trauma and bony surfaces come in contact with each other. This leads to further bone erosion, sometimes leading to osteophytes formation. Arthritis is the most prevalent disease in our society, with a worldwide distribution.4, 5 There is higher prevalence of Osteoarthritis with advanced age and in females.16 Knee osteoarthritis produces significant changes in health related quality of life, particularly physical, mental, and social components of health. The patient usually experiences pain in the knee joint with considerable morning stiffness which may or may not persist during the day time depending on the severity of the disease. The pain increases with any physical activity like climbing or descending the stairs or even during the majority of ADL’s.
There are many treatment approaches formulated to treat this condition. The conservative approaches that are available are strengthening exercises mainly for the quadriceps; stretching exercises to increase the muscle flexibility and range of motion exercises to increase the range of motion of the joint.23 Further, the researchers have also studied the effects of various manual therapy protocols that can be used to treat the condition of Osteoarthritis. Manual therapy has shown beneficial results in managing the arthritic condition, but however the researches concentrating on peripheral joints are very less, as majority of the research is carried out on the spine. Thus, there is an urgent need to carry out the research concentrating on peripheral joints. The purpose of this study is to carry out the research concentrating on peripheral joints. The purpose of this study is to carry out one such research and thus examine the effectiveness of mobilization techniques viz Maitland’s mobilization in improving the pain, stiffness, physical activity and functional independence in the patients with knee joint osteoarthritis.
30 subjects were randomly divided into two groups. Group A received conventional physical therapy, Group B received conventional physical therapy and Maitland’s mobilization. All the two groups were assessed pre and post intervention program for pain (VAS Scale), pain, stiffness, physical activity (WOMAC index). To check the effectiveness of the intervention, comparison between pre and post intervention for all the outcome measures (VAS score and WOMAC score) were done for all the two groups.
Paired samples t test was used to compare the effectiveness between the pre test and the post test measurements of VAS score and WOMAC score all the groups. The subjects of the two groups showed a significant improvement (p<0.001) in pain (shown by VAS scale), pain, stiffness and physical activity (as shown by WOMAC index) after 4 weeks of treatment.
All the groups showed significant improvement in mean values. The pre treatment mean values for Group A were 7.13, 67 for VAS and WOMAC respectively while the post treatment values for the same were 4.93 and 52.66 respectively. In the same way the pre treatment values for the Group B was 7.27 and 65.47 (VAS and WOMAC for Group B). While the post treatment values for Group B was 3.53 and 26.87 (VAS and WOMAC respectively for Group B).
These findings suggest that the protocol of all the two groups is effective in improving pain, stiffness, physical activity and functional independence. Improvement in the VAS score was noted in the two groups. The improvement in the VAS score in the Maitland’s group can be attributed to mobilization techniques used in this group. This corresponds with evidence from spinal mobilization studies which demonstrated improvements in Pressure Pain Threshold (PPT) of approximately 25% and 30% following treatment. It also supports a similar pattern found during peripheral joint mobilization, and a previous study showed that mobilizing sub acute ankle injuries increase PPT 23% more than the manual contact procedure. Paungmali et al. also found that an elbow mobilization with movement technique produced an improvement in PPT 23% more than the manual contact procedure. Thus, both peripheral and spinal mobilizations immediately reduced mechanical hyperalgesia more than control procedures. The enhanced hypoalgesic effect of repetitive mobilization may reflect changes in the local cellular environment.
A recent in vitro study of healthy animal fibroblasts suggested that movement may alter concentrations of inflammatory mediators, known to sensitize peripheral nociceptors. Levels of the prostaglandin PGE2, an inflammatory mediator strongly implicated in arthritic hyperalgesia, were assessed before and after fibroblast cells were subjected to cycles of mechanical deformation, designed to mimic mobilization effects. After 24h, these ‘mobilized’ cells were found to contain nearly 70% less PGE2 than undisturbed control cells. Pain relief, however, is multifactorial and complex. Although mobilization may initiate local physiological mechanisms, additional central mechanisms may also be involved. These central mechanisms could include activation of local segmental inhibitory pathways in the spinal cord, or descending inhibitory pathways from the brainstem. These effects of mobilization along with the other conservative approaches significant improvement noted in the VAS score in these groups.
In the control group of this study which received only conservative management comprising mainly of strength training also reported significant improvements in the VAS score. This results are in accordance with the previous studies which found that strength training reduces pain. Daholin et al. also found that both high and low resistance strength training improved clinical effects in terms of pain, function, walking time and muscle torque.
The other outcome measures of this study were WOMAC index which was used to measure the improvements in physical activity and functional independence respectively, in the patients with knee OA. Improvement in the WOMAC score was also was also found in both the groups. The improvements found in Maitland’s group can be attributed to the immediate effects of knee joint mobilization on motor activity. A previous study reports that there was a clear trend towards the greatest improvement in sit to stand and total ‘up and go’ time following the Mobilization treatment. This improvement may reflect reversal of reflex pain inhibition Additionally, changes in motor activity may be a further indication of a centrally mediated response.
It has been demonstrated that mobilization can enhance motor activity alongside hypoalgesic and sympatho-excitatory responses. Sterling et al. found that cervical mobilization improved deep neck flexor function in subjects with neck pain. Vicenzino et al. also similarly found that cervical mobilization increased pain-free grip in subjects with lateral epicondylalgia, a result which was replicated with a local elbow mobilization with movement intervention. In accordance with our results, Deyle et al. also found significant(p<0.05) improvements in the WOMAC score while comparing the effectiveness of Maitland’s mobilization given in conjunction with conservative treatment protocol to the experimental group, over the control group which received only conservative treatment. The average 4-week WOMAC score improved 52% for the experimental group and 26% for the home exercise group. In this study also the two groups showed significant improvements in all the outcome measures with p<0.001.
The WOMAC score showed significant improvement in the control group as well. This can be attributed to the findings of the study which report that increases in both the flexor and extensor muscle strength increases the knee stability. Enhanced knee stability results in better functional performance of the lower extremity. A previous study concluded that strength training is beneficial for the patients with knee OA. Also the study Daholin et al. found the improvements in WOMAC score and walking distances in the subjects who were given high resistance training exercises.
Mobilization techniques are mainly employed to reduce pain and increase function. Maitland’s mobilization comprises of graded oscillatory movements which are passive in nature. The grades of mobilization that were used in the study were Grade 1 and 2 in acute painful conditions and Grade 3 and 4 to increase the range of motion. Patients who reported acute condition of the joint and had a high level of pain irritability were treated with the Grades 1 and 2. Later on as the pain threshold and tolerance increased the grades of mobilization were progressed to Grades 3 and 4. While the patients who were chronic suffer and had less irritability of pain, the Grades 3 and 4 were used.
Mobilization techniques are thought to produce Neurophysiological effects as it stimulates the mechanoreceptors to decrease the pain and increase the awareness of position and motion because of afferent nerve impulses. Mobilization also improves nutrition of the joint, as distraction or small glinding movement’s causes synovial fluid movement thus enhancing the nutrient exchange. It also improves the mobility of mobilization when combined with conventional exercises could have been produced significant improvements in the subjects in Maitland Group in this study. Similar effects were observed in study conducted by Deyle et. al.
The control Group only received conventional exercises. But still the significant improvements were found in the improvement of both the parameters. Evgenia Dimitrova also found that strengthening of knee musculature was more effective after the MWM and was associated with significant improvement in quadriceps strength and function.49It is well known that the weakness in muscular strength of the patients with knee Osteoarthritis causes reduction in functional performance. Michael et al. concluded that subjects with knee Osteoarthritis had significantly less quadriceps strength relative to BMI. It has shown that quadriceps weakness is common in patients with knee Osteoarthritis and this weakness has been attributed to failure of voluntary activation. Studies also conclude that the magnitude of quadriceps activation failure (QAF) serves to moderate the relationship between quadriceps strength and physical function. Physical function may be more severely affected by the weakness of quadriceps muscle in individuals with knee Osteoarthritis who have higher degree of QAF than those who may have quadriceps weakness but do not have QAF.
Thus, the conventional exercises were mainly designed to strengthen quadriceps and hamstrings, thereby reducing the QAF component and increasing the quadriceps strength and physical function. Thus the significant improvement was reported in the control group over a period of 6 weeks. In addition to the exercises all the two groups also received cryotherapy. Research by Lucie Brosseau et al. suggests that ice massage has a statistically beneficial effect on ROM, function and knee strength. So cryotherapy also a factor helps in reducing the pain in all the subjects.
To compare the effectiveness within the group one way ANOVA and the post hoc Tukey test were used. There was significant difference found between all the groups showing that all treatment protocols had made the improvement. The findings suggest that the control group 1 significantly different in the effectiveness in improving pain, stiffness, physical activity and functional independence when compared with the control group.31, 32
The mean difference in the pain score of Maitland’s Group Vs Control Group is 1.60, showing highly significant difference between them. This shows that pain reduction was highly significant in the Maitland’s group when compared to the other. This can be attributed to the immediate hypoalgesic effects produced by the mobilization procedures.
Thus, the results of the study suggest that experimental group 1 which received conventional exercises and Maitland’s mobilization achieved the achieved the highest improvements in pain, stiffness, physical activity and the functional independence compared to the other groups.
The above results support experimental hypothesis.
When all the two interventions were compared for effectiveness in improving pain, stiffness, physical activity and functional independence Group B which received Maitland’s mobilization and conventional exercise proved more effective as compared to other group.
Limitations
Following are the limitations of our study:
The study was limited to small sample size of 30 subjects with Osteoarthritis of knee joint with 15 in each group.
Sampling technique used was not random. So generalization of the results obtained is not possible.
The study did not include long term follow up. Thus, the results cannot tell us about the effectiveness of all the two interventions in long term basis.
Summary
Osteoarthritis is a common degenerative condition among the elderly. It is characterized. With the damage to the articular cartilage and persists with the symptoms of pain and stiffness in the joint. This study was conducted with 30 patients with Osteoarthritis of knee joint. The subjects were divided into three groups:
Group A comprised of 15 subjects. Patients in this group received conventional physiotherapy comprising of Strengthening exercises, Stretching exercises, Range of motion exercises and cryotherapy.
Group B(Experimental Group 1) comprised of 15 subjects. Patients in this group received Maitland’s Mobilization and Conventional physiotherapy exercises.
All the subjects were assessed pre and post intervention program for VAS scale and WOMAC scale test. After analyzing the data following conclusions were drawn; Results showed that there was significant improvement in the VAS score and WOMAC score of all the two groups for the pre and the post test measurement. The inter group comparison of all the two groups showed that there was highly significant difference between the Maitland’s group and the control group (p<0.001).
Conclusion
Major findings observed in our study are:
Significant improvements in terms of all the outcome measures were found in the two groups.
Significant differences between all the two groups were found. In the experimental groups, i.e. Maitland group achieved better results in terms of pain, stiffness, physical activity and functional independence when compared with the control group.
We conclude that conventional exercises when combined with Maitland’s Mobilizations are effective in improving pain, stiffness, physical activity and functional independence in patients with knee joint osteoarthritis.
Abbreviations
ADL: Activities of daily living
AP Mobilization: Anteroposterior Mobilization
MVIC: Maximum voluntary isometric contraction
NSAID: Non Steroidal Anti Inflammatory Drugs
OA: Osteoarthritis
PFPS: Patellofemoral Pain Syndrome
PG: Proteoglycans
PPT: Pressure Pain Threshold
QAF: Quadriceps Activation Failure
VAS: Visual Analogue Scale
WOMAC: Western Ontario and McMaster Universities